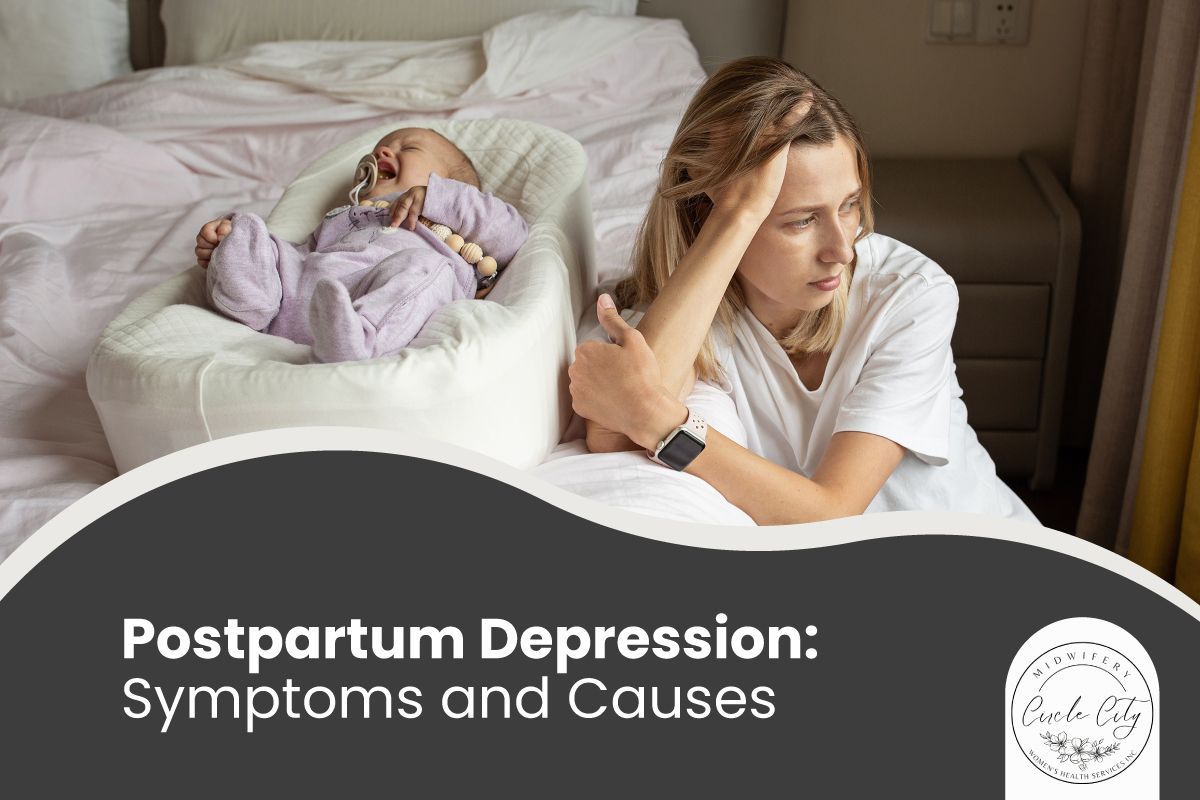
Becoming a new mother is one of life’s most rewarding experiences. But for some women, the joy of motherhood can be overshadowed by feelings of sadness, anxiety, and exhaustion. This may be due to
postpartum depression (PPD), a common but serious condition that affects new mothers.
At
Circle City Midwifery, we aim to support mothers by providing care, guidance, and resources to navigate postpartum challenges.
What is Postpartum Depression?
Postpartum depression is more than just feeling “a little down” after giving birth. It is a medical condition that can affect a mother’s emotional well-being, her ability to care for herself, and her bond with her baby. Symptoms can appear within the first few weeks after delivery and may persist for months if left untreated.
Baby Blues vs. Postpartum Depression
It’s normal for new mothers to experience the
baby blues—mild mood swings caused by hormonal changes. However, baby blues usually resolve within
two weeks.
Symptoms of Baby Blues:
- Mood swings
- Irritability
- Crying spells
- Temporary sadness
Postpartum depression is different. Symptoms are more intense, last longer, and may require professional treatment.
Common Symptoms of Postpartum Depression
Recognizing PPD early is essential. Signs may vary, but often include:
- Persistent sadness or irritability
- Loss of interest in daily activities
- Trouble bonding with your baby
- Changes in sleep patterns—insomnia or excessive sleeping
- Changes in appetite
- Overwhelming fatigue
- Difficulty concentrating or making decisions
- Intense feelings of guilt, worthlessness, or inadequacy
- Thoughts of self-harm or harming the baby
Important: If you experience thoughts of harming yourself or your baby, seek help immediately.
What Causes Postpartum Depression?
There is no singular underlying cause for postpartum depression. Instead, it's likely the result of a combination of physical, emotional, and environmental factors.
Postpartum depression causes can include the:
Hormonal changes
After childbirth, a mother's hormone levels, particularly estrogen and progesterone, drop significantly. This
sudden hormonal shift can contribute to mood instability and the development of postpartum depression.
Genetic predisposition
Mothers with a family history of depression or other mood disorders may be more susceptible to developing postpartum depression, suggesting that there may be a link to the condition.
Environmental stressors
Caring for a newborn can be an overwhelming experience, particularly for first-time mothers who are grappling with the physical and emotional demands. Sleep deprivation, social isolation, and a lack of support from friends and family can exacerbate anxiety and depression following delivery.
Birth complications
Complications during
labor and delivery, such as an emergency C-section, premature birth, or a baby with health problems, can increase the risk of postpartum depression due to added stress and anxiety.
Breastfeeding difficulties
Mothers who experience difficulties breastfeeding, such as problems with latching or low milk supply, may be more prone to postpartum depression due to guilt, frustration, and inadequacy.
Personal history
Individuals with a history of abuse, depression, anxiety, or other mental health conditions are at a higher risk of developing postpartum depression.
Diagnosing Postpartum Depression
Healthcare providers use several approaches to diagnose PPD:
- Screening tools – Beck Depression Inventory (BDI), Edinburgh Postnatal Depression Scale (EPDS), Postpartum Depression Screening Scale (PDSS)
- Symptom criteria – Symptoms must last
at least two weeks, including sadness or loss of interest in activities
- Excluding other conditions, – Postpartum anxiety or psychosis may present similar symptoms
Treatment and Support for Postpartum Depression
Treatment and support can help mothers recover and enjoy motherhood. Common options include:
- Therapy: Cognitive Behavioral Therapy (CBT) and Interpersonal Therapy (IPT) help manage negative thoughts and build coping skills.
- Medication: Antidepressants, especially SSRIs, can regulate mood. Your provider will recommend safe options if you’re breastfeeding.
- Support groups: Connect with other mothers online or in your community. Sharing experiences reduces isolation.
- Lifestyle changes: Regular exercise, healthy eating, proper sleep, and self-care improve emotional well-being.
- Social support: Family and friends can assist with childcare and provide emotional encouragement.
- Professional support: Doulas, lactation consultants, and postpartum nurses offer guidance during the postpartum period.
- Hormone therapy: In some cases, estrogen therapy may be prescribed to help balance hormones.
Your Mental Health Matters - Seek Help for Postpartum Depression
Motherhood can be both rewarding and challenging, but it's essential to prioritize your mental health along the way. If you're experiencing symptoms of postpartum depression, don't hesitate to seek help. Our team at
Circle City Midwifery is here to support you every step of the way. Contact us today at 951-547-4208 or email
info@ccmidwifery.com to find out more about our services and how we can help.